The redesigned Children and Youth with Support Needs system announced on February 10, 2026, introduces two new direct-funding streams—BC Children and Youth Disability Benefit and BC Children and Youth Disability Supplement—plus an expansion of diagnosis-free community-based services over a multi‑year rollout. It also abandons autism funding that provided $6k funding per year to beneficiaries, regardless of autism functioning labels. When a decision like this happens and 1000s of parents flip out, seeing badly needed resources revoked, I get curious about what the original inputs from interest holders were into the decision. You can read them: https://www.bcdisabilitycollab.ca/mcfd . This is my gist, from a very rapid review.
What stakeholders universally called for
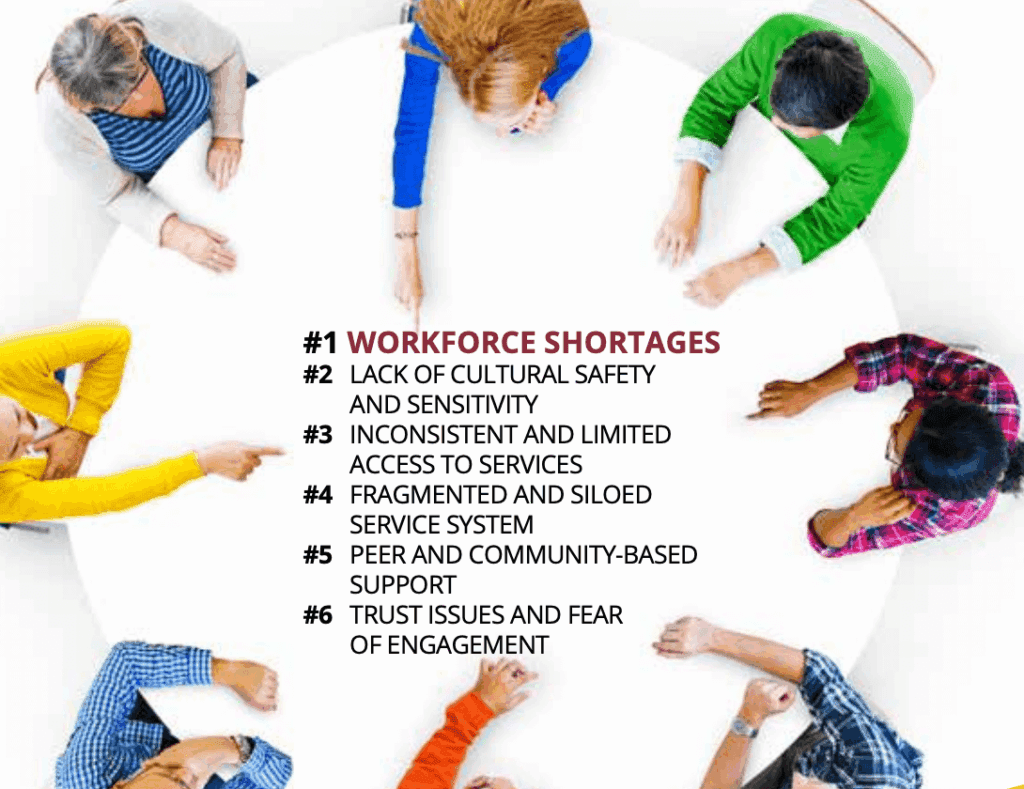
Across every report—from community-led engagement across 23 BC communities to clinical submissions from therapy associations, to lived-experience testimony from families raising children with complex medical needs—several core demands emerged with striking consistency.
BC Association for Child Development and Intervention (BCACDI)
BC’s CYSN Service Delivery Transformation – Position Paper
- Advocates for building on existing network of community-based non-profit Child Development Centres rather than disrupting proven services through procurement
- Calls for transparent funding formula based on population data and prevalence rates, with sufficient equitable funding indexed to inflation
- Proposes hybrid model maintaining individualized autism funding while implementing needs-based behavioural support contracts through community agencies
- Emphasises multi-disciplinary team-based approaches leveraging CARF-accredited organisations’ existing expertise, community relationships, and family-centred practice
- Recommends robust human resources strategy including provincial recruitment lead, increased training seats for therapists, standardised wage grids across sectors
Individual funding has been in place in BC for children and youth with Autism for almost two decades, and is also available for some families of school aged children that qualify for certain programs. BCACDI acknowledges that for some this model works well, and doesn’t believe in taking anything away from families currently accessing funding in this manner. — BC Association for Child Development and Intervention (BCACDI)
BC Complex Kids Society
- Documents how 5,000+ children with medical complexity represent nearly 30% of paediatric healthcare costs but receive fragmented, chronically underfunded support unchanged since 1980s
- Calls for rights-based, needs-based funding assuring every family access without waitlists, with family-by-family approach budgeted on evolving demand
- Proposes community-based care coordination teams with nurse key workers as single point of contact, integrated across health, education, social services
- Recommends Caregiver Benefit (up to $1,500/month like Quebec) or Certified Nursing Assistant program compensating family caregivers for specialised labour
- Advocates for funding home and vehicle accessibility, portable services across regions, extended support to age 25, trauma-informed culturally safe practices
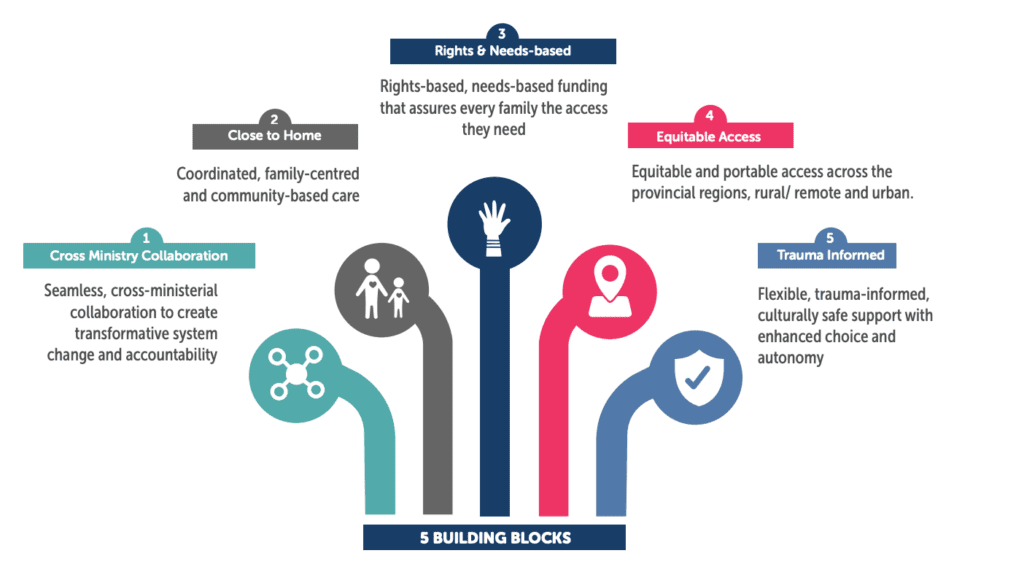
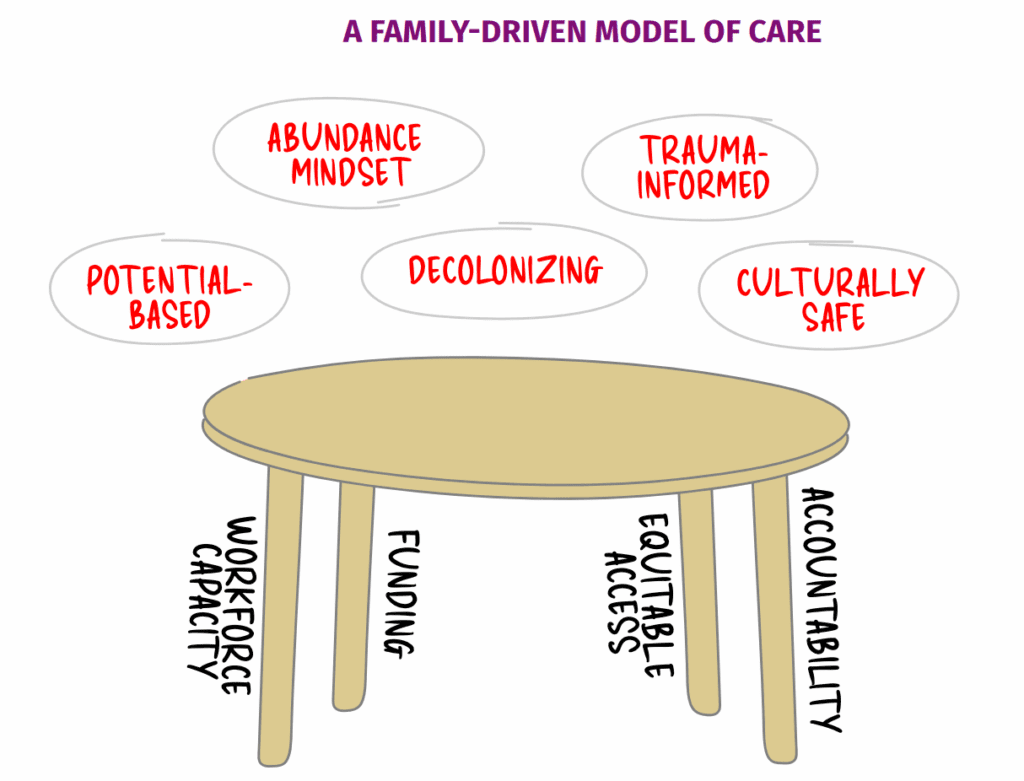
BC Disability Collaborative
A Family-Driven Model of Care: Setting the Table for Disability Rights in BC
- Calls for family-driven care model centred on potential-based, abundance mindset, decolonised, trauma-informed, and culturally safe values
- Demands adequate sustained funding with transparent formulas, quality workforce capacity, equitable access regardless of diagnosis or location
- Advocates for human rights complaint recognising BC’s current treatment of children with disabilities violates Charter rights and UN Convention on Rights of Persons with Disabilities
- Proposes unified “I am one of them” campaign highlighting 80,000+ children excluded from services annually
Community-Led Collaboration Project
Invest in Communities: 11 Calls to Action
- Represents engagement of 2,010+ people across 23 BC communities in community-driven conversations about needed supports
- Calls for cultural safety prioritizing Indigenous, newcomers, refugees; fund translation services and cultural liaison workers
- Demands adequate responsive funding based on community needs, population growth, geographic considerations
- Advocates for flexible respite meeting unique family needs, eliminating therapy waitlists through workforce recruitment
- Emphasises access to mental health supports, inclusive child care, meaningful education with supported teaching teams
“Over two years, more than 130 organizations across B.C. came together to speak with over 2,000 people about their experiences and ideas when it comes to supports and services for children and youth with disabilities and support needs.
The result of these conversations is two-fold: a vision for all children and youth to achieve their fullest potential and thrive in community, and 11 calls to action with specific recommendations to make this vision a reality.”
Down Syndrome Resource Foundation
- Documents that children with Down syndrome receive no financial or therapeutic support based on diagnosis alone despite universal need
- Demonstrates value of specialized support: 93.1% of families identified Down syndrome-specific knowledge as critical to success
- Calls for funding beginning at birth for all individuals with Down syndrome, continuing across lifespan without arbitrary cutoffs
- Recommends hybrid model allowing family choice between individualised funding or centre-directed funding through DSRF
- Advocates for specialised services incorporated into schools, addressing inadequate educational support reported repeatedly
Family Support Institute of BC & UBC Canadian Institute for Inclusion and Citizenship
Family Voices Project: Report of Community Engagement
- Documents how families must become expert advocates, navigators, and case coordinators just to access fragmented services, with devastating impact on family wellbeing
- Emphasises need for family agency, choice and control through individualised funding models that allow families to select providers and determine service timing
- Calls for systemic change including reduced social worker caseloads, inter-ministerial coordination, navigator roles independent of ministry gatekeeping
- Highlights geographic inequities leaving rural families without services, cultural safety gaps for Indigenous families fearing child protection surveillance, and need for needs-based rather than diagnosis-based eligibility
- Recommends family-centred approach supporting entire household including siblings and caregivers experiencing burnout
FSI did research with 46 individuals around the province. Families described painful impacts of fragmented CYSN systems: emotional/financial strain navigating complexity, waitlists, advocacy burdens. Indigenous and equity-deserving communities face culturally unsafe services compounded by colonial legacies. Participants demand family-centred investment including caregiver/sibling supports, trust-building, choice/control, adequate funding, workforce capacity addressing rural/urban shortages, coordinated cross-ministry continuity from early intervention through adult transitions, navigator roles reducing navigation burden.
Health Sciences Association of BC
Building on What Works – Child Development Centres and the Future of CYSN Services
- Calls to stop competitive tendering/RFPs that risk privatisation, immediately increase CDC funding by 50% minimum
- Documents moral distress and burnout from grossly inadequate staffing: 0.7 FTE OT for 120 children, 1.0 FTE SLP for 140 children
- Advocates enshrine not-for-profit delivery in legislation, move CDCs to Ministry of Health, develop population-based funding formula
Physiotherapy Association of BC
MCFD Children and Youth with Support Needs Engagement Project
- Highlighted the central role of early, consistent therapy access (e.g., physiotherapy) in maintaining developmental gains, warning that funding instability risks regression and increased long-term need.
- Emphasised that service delays and waitlists worsen when funding becomes pooled or centrally allocated, disproportionately affecting children with complex or evolving physical needs.
- Identified the importance of clinically driven decision-making (not administrative caps) to determine therapy intensity, reinforcing family concerns about loss of individualised funding flexibility.
- Stressed that families require predictable funding continuity to maintain therapeutic relationships and progress, especially for children with lifelong physical disabilities.
- Noted that effective outcomes depend on interdisciplinary coordination (physio, OT, speech, school supports), which can fragment when funding is reorganised across agencies.
- Raised concerns that changes to funding structures must not undermine function, mobility, and participation goals, which families consistently prioritise for quality of life.
- Reinforced that equitable access requires geographic parity, since rural families already face limited therapist availability and would be further disadvantaged by centralised funding controls.
Reciprocal Consulting
- Brought forward the voices of underserved communities (immigrant, Indigenous, Deaf/Blind, LGBTQ2S, newcomer families), showing how rigid funding models compound existing barriers to access.
- Identified strong demand for individualised funding options beyond autism, particularly to support respite, interpreters, and inclusive programming that pooled models often fail to cover.
- Highlighted the need for culturally safe, trauma-informed, and neurodivergent-affirming services, stressing that funding structures must allow families to choose providers who meet these needs.
- Documented that lack of funding flexibility leads to caregiver workforce exit, as parents reduce employment when adequate supports and respite are unavailable.
- Emphasised that families want navigation help and coordinated systems, not fragmented program silos that require repeated applications when funding streams change.
- Identified widespread calls for expanded local programming and community connection, noting isolation increases when families cannot allocate funding to social and developmental supports.
- Demonstrated that equity requires funding approaches that recognise intersectionality and access barriers, rather than assuming one uniform service model fits all families.
Interest holder input vs final decisions
Across the interest holder engagement reports published during the 2023–2024 consultation window, several “high-consensus” asks appear meaningfully reflected in the final design: (a) a shift toward functional-needs framing, (b) hybridised funding administration options (direct payment / invoicing / agency‑coordinated), (c) expanded navigation/family support (planned), and (d) province-wide expansion of free community-based services without requiring a diagnosis.
At the same time, multiple interest holder recommendations are only partially addressed or remain unspecified in binding policy text, including: transparent funding formulas indexed to inflation and cost of living; enforceable wait-time/access standards with public reporting; durable governance/accountability mechanisms beyond audits; and concrete workforce strategies that address pay, training seats, rural recruitment, and service quality.
The largest, evidence-backed divergence points in the written policy record are: (a) the planned termination of Autism Funding Program by March 31, 2027, despite numerous interest holder voices urging maintenance/expansion of individualised autism funding; (b) the Disability Supplement’s dependence on eligibility for the federal Disability Tax Credit, introducing clinician/administrative gatekeeping for that stream; and (c) the explicit thresholding of the Disability Benefit to “the highest” needs—illustrated in the Children and Youth with Support Needs: Guide for Current Service Recipients—leaving some children with real disabilities to rely primarily on community services and/or the DTC‑linked supplement.
Overall, interest holder input was not “largely ignored,” but it was selectively incorporated: core architectural elements align with many interest holder themes, while several structural equity, governance, and long-horizon continuity asks (e.g., caregiver compensation, supports beyond age 19/25, enforceable access standards, and insulation from medical/CRA gatekeeping) are either absent from current policy texts or deferred as “to be developed.”
Scope and methodology
This analysis follows the Province’s documented engagement window (“From March 2023 through December 2024”) and compares interest holder recommendations hosted by the Province against the policy design published on February 10, 2026 and associated transition documentation.
Key actors and acronyms used below (named once here for clarity): Ministry of Children and Family Development (MCFD); Canada Revenue Agency (CRA); Representative for Children and Youth (RCY); BC Disability Collaborative (BCDC); Family Support Institute (FSI); BC Association for Child Development and Intervention (BCACDI); BC Complex Kids Society (BCCK); Down Syndrome Resource Foundation (DSRF); Health Sciences Association (HSA); At Home Program (AHP).
Method steps applied consistently:
- Identify explicit interest holder “calls to action,” “recommendations,” or “goals” in interest holder reports hosted on gov.bc.ca
- Extract the corresponding final-design rule or commitment from official sources: the Feb 10, 2026 news release, the main CYSN redesign pages, and the Guide for Current Service Recipients
- Assign a status per demand: Fully Met / Partially Met / Not Met / Unclear, based strictly on what is written in those official texts (not on anticipated implementation success)
- Add a “family implications” note emphasising gatekeeping (diagnostic/functional assessments, clinician attestations, DTC), rural access, administrative burden, and continuity risks
Limitations (explicitly flagged):
- No public, official meeting minutes or decision logs were located within the consulted sources; where a governance detail appears absent, it is marked unspecified rather than assumed
- No evaluation reports for the new Benefit/Supplement were located (the redesign is newly announced and begins phased implementation in 2026)
- The user-provided outline and three attached articles were treated as interpretive context and cross-checks, not as primary evidence of government decisions
What interest holders asked for
The Province’s CYSN community engagement page lists multiple community partner reports and proposals submitted to inform a redesigned service model. Across these reports, recurring “core asks” show striking convergence—especially needs-based support, reduced administrative burden, culturally safe services, navigators, workforce capacity, and dependable access to therapies/respite close to home.
Interest holder demands most directly relevant to your requested focus areas can be grouped as follows (each is then assessed demand-by-demand in the matrix below):
- Eligibility and fairness: move away from diagnosis-only gatekeeping toward function/needs, while avoiding new exclusion thresholds that leave many families unsupported
- Hybrid funding and real choice: keep (and expand) individualised funding options while strengthening publicly funded community-based services, recognising that different families prefer different administrative burdens and delivery modes
- Access enablers: navigation roles, simplified paperwork, coordinated records/portals, and inter-ministerial coordination so parents aren’t forced into full-time “case management”
- Continuity and long-horizon supports: several interest holders—especially those representing medical complexity and some disability-specific communities—asked for continuity beyond childhood cutoffs (often to age 25 and/or across the lifespan)
- Workforce and capacity: expand training seats, address wage inequities, recruit/retain providers, and set measurable access standards (including public reporting)
- Equipment, supplies, and home/vehicle modifications: streamline and adequately fund medical equipment/supports and accessibility adaptations, recognising the practical realities of caring for complex kids at home
What government decided and documented
The official design, as published February 10, 2026, has three major pillars:
First, the Disability Benefit is described as direct funding for ages 0–19 with “significant and/or complex support needs” and provides tiered annual amounts ($6,500 base, up to $17,000 higher tier). MCFD frames eligibility as based on “support needs” rather than income and “not just” diagnosis, but it implements two pathways: a Direct Admit pathway explicitly tied to specified diagnoses/clinical thresholds and a Needs-Based Review pathway relying on functional assessment and/or “health-care provider attestation.”
Second, the Disability Supplement is an income-tested cash benefit starting July 2027 that is automatically delivered via CRA if the child is approved for the federal DTC (and the family meets income/tax filing conditions). This design choice is central for gatekeeping analysis, because DTC eligibility requires certification by a medical practitioner and CRA approval, and the Guide notes that providers may charge fees to complete the form.
Third, community-based services are explicitly expanded over the next three years, with eligibility stated as ages 0–18 and “No diagnosis is required,” and a phased rollout of priority service areas (pediatric therapies Spring 2026; behavioural/mental health Summer 2027; navigation/family support Winter 2027; 6–18 programming Spring 2028).
Transition and continuity commitments are prominent in the Guide for Current Service Recipients: existing supports remain in place until families are “successfully transitioned,” Autism Funding invoices continue through March 31, 2027, and AHP medical equipment/supplies remain unchanged. Yet the Guide also illustrates an explicit “Benefit eligibility threshold” (e.g., “Ollie does not qualify for the… Benefit”) while pointing him toward early intervention supports and a DTC-linked pathway.
Demand-by-demand assessment
Annotated checklist of high-sensitivity interest holder asks
| High-sensitivity ask theme | Indicator | Concise rationale (evidence-backed) |
|---|---|---|
| Needs-based in principle | ~ | Official language emphasises needs/function, but Direct Admit is diagnosis/threshold-based and Needs-Based Review depends on clinical attestation/assessment per the Disability Benefit page. Supplement depends on having Disability Tax Credit (DTC) |
| Hybrid funding administration (true choice of pathways) | ✓ | Benefit has three administration pathways (direct, invoicing, agency‑coordinated) are explicitly offered and may be combined. Supplement is cash benefit that can be spent on anything. |
| Free community services without diagnosis | ✓ | Expanded community-based services explicitly state “No diagnosis is required” (ages 0–18). $80 million in new funding over 3 years. Lack of clarity whether this will merely expand existing programs or reduce waiting times or genuinely add services for underserved populations, e.g. PDA focused services, more services for people in remote communities. |
| Autism individualised funding continuity long-term | ✗ | Autism Funding ends March 31, 2027 / April 1, 2027 replacement, despite interest holder calls to maintain/improve individualised autism funding. |
| Gatekeeping minmilsed | ✗ | The Disability Supplement is explicitly contingent on DTC approval and medical practitioner certification. Benefit restricted to certain diagnoses, unless you request review path which has more testing. |
| AHP medical equipment/supplies continuity | ✓ | Official pages and the Guide state AHP medical equipment/supplies “remain unchanged” |
| Caregiver compensation (e.g., caregiver benefit / paid caregiver model) | ✗ | No caregiver wage/benefit policy appears in Benefit/Supplement/community services documentation |
| Supports beyond age 19/25 | ✗ | Disability Benefit is limited to age 19; expanded community services to 18; no extension to age 25 appears in official docs |
| Transparent funding formula (inflation/cost-of-living indexed) | ? | Government commits to “shared transparently” criteria for benefit-level determinations but does not publish a formula or indexation mechanism in the consulted texts |
| Wait-time standards and public reporting | ? | Interest holders call for standards/reporting; official docs emphasise reducing wait times but do not specify measurable standards or reporting mechanisms |